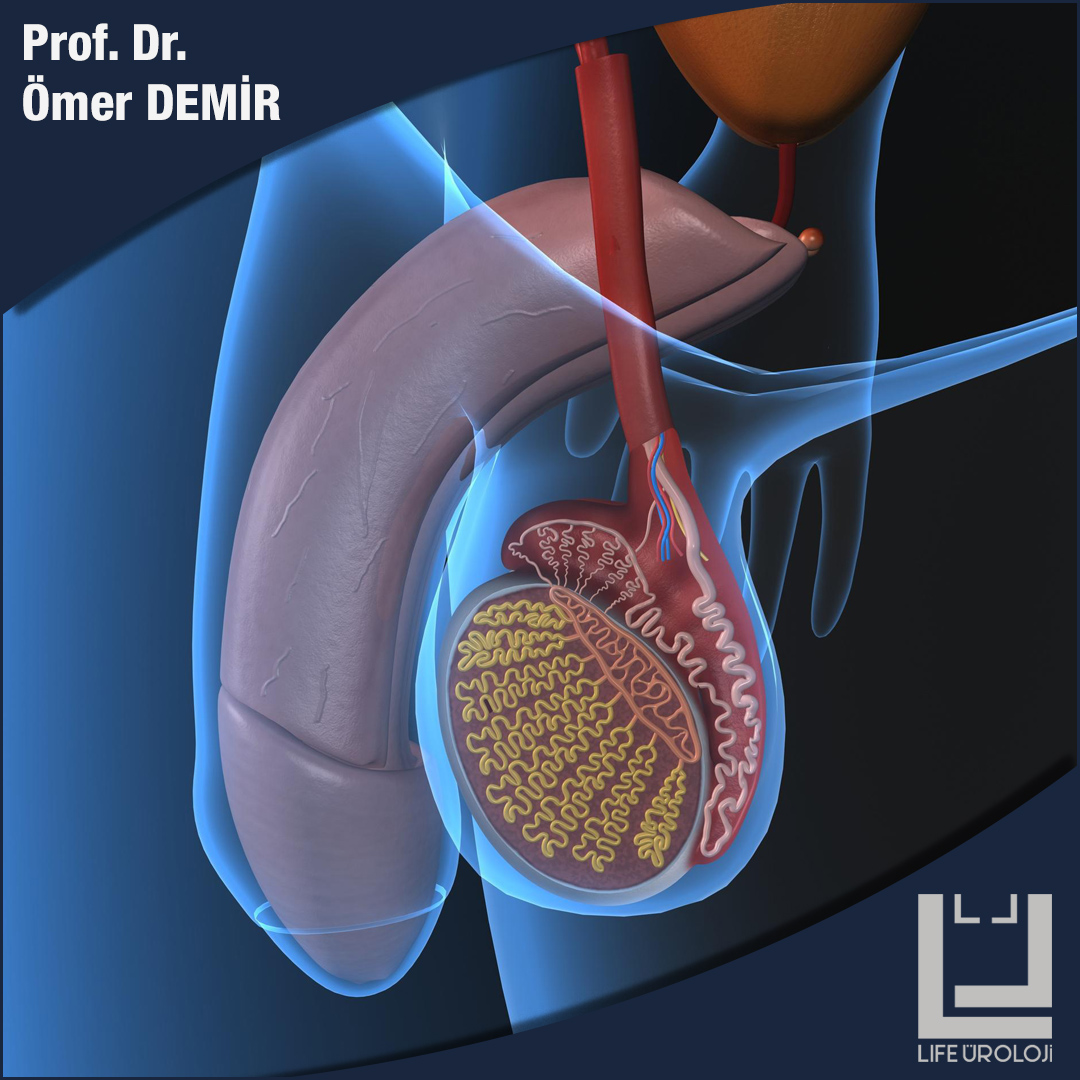
TESTICULAR CANCER
Testicular cancer is the most common cancer arising from the testicles in men aged 15-44. However, testicular cancer may rarely occur before puberty.
Symptoms
The most common first noticed symptom of testicular cancer is a painless lump in the testicle. The lump is usually painless, but some people notice some pain or discomfort coming from the affected testicle. Not every bump and lump in the scrotum is cancer. Swelling in the scrotum may also occur in cases such as inguinal hernia, hydrocele, sperm duct cysts and varicocele. However, when a swelling or lump is noticed in the testicles, it is necessary to consult a doctor as soon as possible for early diagnosis. Because early diagnosis is the most important factor that increases treatment success in testicular tumor.
Risk factors
Certain risk factors increase the likelihood of developing testicular cancer. These are: Race and ethnicity; Testicular cancer risk in white men is approximately 4 to 5 times higher than African and Asian men. Family history; Siblings and sons of men with testicular cancer are also at risk. Undescended testicles; The testicles develop in the abdomen and usually move down (descend) into the scrotum before birth.
Some babies do not descend into one or both testicles at birth. This situation can be corrected by surgery. There is a large increased risk in men whose undescended testis has not been surgically corrected. Men who had undescended testicles corrected as a baby are still at risk.
Infertility; Infertile men with abnormal sperm count have a slightly higher risk of developing testicular cancer than in the normal population.
Diagnosis
Examination of the testicle and subsequent ultrasound examination in the presence of a lump in the testicle will confirm the diagnosis. Ultrasound is a simple, painless test that uses sound waves to view the testicles. This test can tell whether the lump is a solid mass (possibly a tumor) or a noncancerous (benign) cyst (a fluid-filled lump common in the testicles). In addition, a blood test should be performed to evaluate alpha-fetoprotein (AFP), beta human chorionic gonadotropin (beta-hCG) and lactic dehydrogenase (LDH) levels in order to evaluate some of the increased markers in testicular tumor.
Treatment
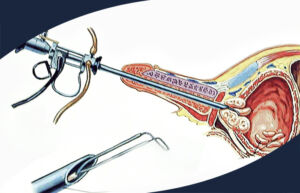
If cancer is diagnosed, the affected testicle must be surgically removed. The testicle is removed from the groin area with an incision made in a size varying according to the size of the mass. In some special cases and when the mass in the testicle is very small, only the tumor can be removed by protecting the healthy part of the testicle. The removed testicle is sent for pathological evaluation to be examined under a microscope to confirm cancer.
Sex life is usually not affected if only one testicle is removed. Erectile function, male hormone level and chance of having a child are not affected negatively. However, because the testicular tumor has spread, if additional chemotherapy or radiotherapy is given, it can negatively affect the chances of having a child. However, it is observed that many patients return to normal spermiogram values one year after receiving chemotherapy or radiotherapy treatment.
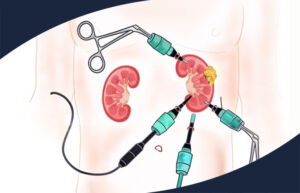
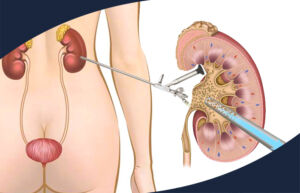
If a diagnosis of testicular cancer is confirmed, further testing is usually recommended to assess whether the cancer has spread. This assessment is called cancer staging. Staging aims to determine whether cancer has spread to lymph nodes, lungs, and other organs in the abdomen. Determining the stage of your cancer helps your doctor suggest the best treatment options for you.
Tests to be recommended for cancer staging include computed tomography (CT) scanning, magnetic resonance imaging (MRI), PET imaging, or other tests.
Treatment in Advanced Testicular Cancer
If testicular cancer has spread to the abdominal lymph nodes, lungs, or other organs, treatment options that may be recommended include surgery, chemotherapy, and radiotherapy. The treatment recommended for each patient will vary depending on various factors such as the stage of the cancer, the type of cancer (seminoma or non-seminoma), and general health status.
Treatment of testicular cancer is usually successful, although it is more likely if it is caught at an early stage. More than 95% of the patients can be treated successfully.
Post Treatment Follow-up
Normally, regular follow-up is necessary after successful treatment to check if the cancer has recurred. These follow-ups can include blood tests and imaging tests such as CT, MRI, and PET.